Intraoperative blood salvage, also known as autologous blood salvage, is a medical procedure involving recovering blood lost during surgery and re-infusing it into the patient. Blood salvage is performed during surgical procedures when the risk of significant blood loss is expected. The recovered blood is collected, processed, and readministered to the patient, decreasing or preventing the need for allogeneic (from a donor) blood product administration. If the blood is not given to the patient, it will be discarded.
Administration of the patient's own blood eliminates the risk of transfusion-transmitted viral disease and transfusion reactions. Patients with multiple red blood cell antibodies or rare blood types benefit by blood salvage during the perioperative (during surgery) and postoperative period. Shortages of rare blood types can put the patient at risk for cardiovascular collapse caused if hemorrhage occurs during the surgical procedure.
Some Jehovah's Witnesses patients refuse allogeneic blood donation. Blood salvage provides an opportunity for autologous blood donation for these patients. Certain modifications in collection technique make autologous blood donation an acceptable treatment for members of this faith.
Pre-operative procedures
Pre-operative blood salvage can be performed prior to the surgical incision during the induction of anesthesia. This blood is collected to be administered post-operatively, because the clotting factors and platelets are protected from activation and destruction caused by the surgery. This procedure is most often used if cardiopulmonary bypass (use of a heart-lung machine) will be instituted. If the blood is not given to the patient, it will be discarded. Pre-operative blood donation or autologous blood donation is a coordinated donation process planned prior to a scheduled surgical procedure, but it is not considered blood salvage.
Peri-operative blood salvage
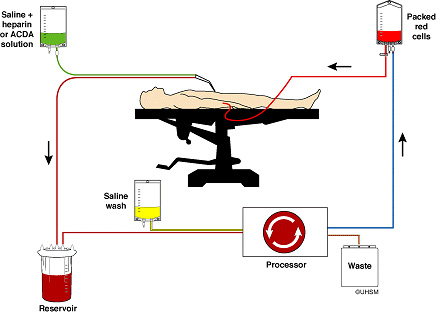
During surgery, the surgeon uses suction in the surgical cavity to collect blood. Anticoagulant is mixed with the blood at the tip of the suction apparatus. The blood is filtered as it is collected into a container. From this collection container the blood may be placed into a transfusion container for direct administration to the patient. This blood will be anticoagulated and will contain all plasma proteins, including activated clotting factors and platelets. More commonly, the blood is processed by centrifugation. The blood is centrifuged to separate the red blood cells from the plasma. The plasma is removed as saline enters the centrifuge to wash the blood. Washing the blood removes anticoagulation, plasma-free hemoglobin, and plasma proteins, including activated clotting factors and platelets. This product is called washed packed red cells. After washing is complete, the blood is collected into a transfusion container free of anticoagulant since all clotting factors have been removed during washing. The container is properly labeled for the patient and clearly marked "AUTOLOGOUS DONOR." The blood can be stored for six hours if refrigerated, and will be destroyed if not used within that time.
Cell processors and salvage devices that wash and save red blood cells, i.e. "cell washers" or RBC-savers:
The basic function is as follows: At the “business end,” where the surgeon is making incisions, a technician will suction the blood out of the surgical field using a special type of suction tube, somewhat like the implement the dentist’s assistant uses to suck the fluid out of the patient's mouth when the dentist is drilling. Instead of the aspirated blood simply being flushed down a sink, however, it passes through tubing and is collected in a reservoir. At the same time as the suction occurs, an anticoagulant is introduced into the line. When enough blood has been collected in the reservoir it is sent to the cell salvage machine, resembling in no small way a washing machine/spin drier. The blood is filtered, then spun in a centrifuge, causing the RBCs to separate from the plasma and stick to the sides of the centrifuge bowl. The plasma goes into a waste bag, and a wash fluid (0.9% normal saline) is introduced into the machine to remove platelets and debris. The washed RBCs are then pumped up to a transfusion bag from where they are returned to the patient through an IV in the usual way.
Direct transfusion
Direct transfusion is a blood salvaging method associated with cardiopulmonary bypass (CPB) circuits or other extracorporeal circuits (ECC) that are used in surgeries, such as coronary artery bypass grafts (CABG ), valve replacement, or surgical repair of the great vessels. Following bypass surgery the ECC circuit contains a significant volume of diluted whole blood that can be harvested into transfer bags and re-infused into the patient. Residual CPB blood is fairly dilute ([Hb] = 6–9 g/dL; 60–90 g/L) compared to normal values (12–18 g/dL; 120–180 g/L) and can also contain potentially harmful contaminants, such as activated cytokines, anaphylatoxins, and other waste substances that have been linked to organ edema and organ dysfunction, both of which require a diuretic to reverse.
Ultrafiltration of whole blood
Hemofiltration or ultrafiltration devices filter the patient's anticoagulated whole blood. The filter process removes unwanted excess non-cellular plasma water, low molecular weight solutes, platelet inhibitors, and some particulate matter including activated cytokines, anaphylatoxins, and other waste substances through hemoconcentration; thus making concentrated whole blood available for reinfusion. Hemofilter devices return the patient's whole blood with all the blood elements and fractions including platelets, clotting factors, and plasma proteins with a substantial Hb level. These devices do not totally remove the potentially harmful contaminants that can be washed away by most RBC-savers. However, the contaminants that are potentially reduced by using RBC-savers, as shown by data from in vitro laboratory tests, are transient and reversible in vivo with hemostatic profiles returning to baselines within hours. The key is that coagulation and homostasis are immediately improved with the return of concentrated autologous whole blood.
Postoperative blood salvage
Postoperative blood salvage is used to remove shed blood from the surgical cavity that has been closed at the completion of the surgical procedure. At wound closure, a catheter is left in the cavity and penetrates the skin for connection to the collection reservoir. If the blood is collected from the chest cavity, no anticoagulation is required. If the blood is collected from a joint, it must receive anticoagulation during collection. The blood from the chest cavity is usually reinfused without additional processing, but may be washed. Blood collected from a joint must be washed prior to infusion. Washing involves centrifugation of the blood to separate the red blood cells from the plasma. In the plasma are the anticoagulant-free hemoglobin and plasma proteins, including activated clotting factors and platelets. Once the red blood cells and plasma are separated, saline is introduced to the centrifuge to displace the plasma with the end product collected into a transfusion container. The final product is called washed packed red blood cells. The container is properly labeled for the patient and clearly marked "AUTOLOGOUS DONOR." The blood can be stored for six hours if refrigerated, and will be destroyed if not used within that time.
Sources - Wikipedia - http://www.surgeryencyclopedia.com - http://www.noblood.org/content/intraoperative_blood_salvage-209 - Case study: http://ether.stanford.edu/library/liver_anesthesia/LDLT%20blood%20loss… Image Credits: - Http://msnbcmedia4.msn.com/j/MSNBC/Components/Slideshows/_production/ss-100805-blood/ss-100804-blood-01.grid-6x2.JPG - Http://www.ebme.co.uk/arts/cell_salvage/2.jpg