World Health Organization (WHO) has been planning and adopting several measures to ensure that equity of care is never compromised or ignored in the delivery of healthcare.
WHO defines equity of care as (source WHO website page on Equity in Health Systems) “Equity is the absence of avoidable or remediable differences among groups of people, whether those groups are defined socially, economically, demographically, or geographically. Health inequities therefore involve more than inequality with respect to health determinants, access to the resources needed to improve and maintain health or health outcomes. They also entail a failure to avoid or overcome inequalities that infringe on fairness and human rights norms. Reducing health inequities is important because health is a fundamental human right and its progressive realization will eliminate inequalities that result from differences in health status (such as disease or disability) in the opportunity to enjoy life and pursue one's life plans”
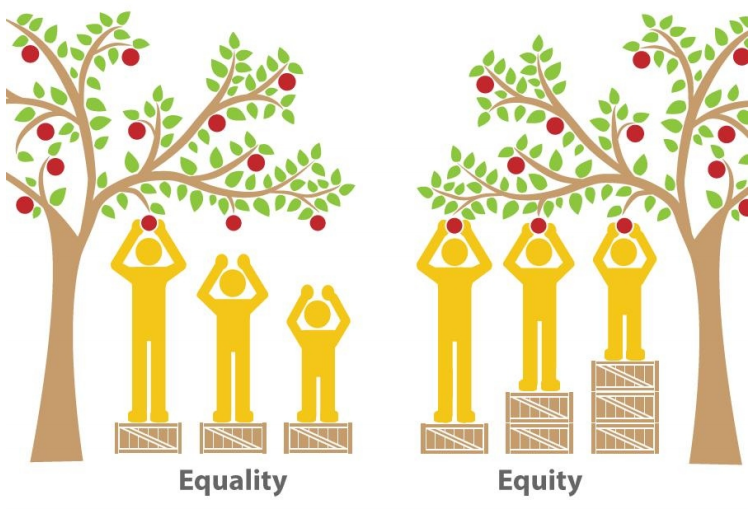
It must be noted that equity of care does not necessarily simply mean giving everybody equal opportunity .Equity is about promoting fairness. The aim of equity is to achieve equality in outcome not in the method to achieve it. In health promotion equity revolves around the achievement of a good level of health for all, which means that each person is given the same amount of control over their own health in order to achieve good health.
Attaining equity of care in a resource constrained and overburdened healthcare system in India is extremely challenging. At most places there seems to be a complete lack of sensitization on the part of healthcare professionals towards such equity measures. This is especially true in the pubic healthcare systems. Whenever the government or enforcement authorities have taken steps to act on this, it has either been that the model is not sustainable or not wholesome and therefore lacking in quality. Individuals with access to good financial resources will always approach the private establishments, while the poor will continue to struggle. Consequently, the availability of better care and cure opportunities is directly dependent upon the social, economical status of the patient. A bigger disadvantage and problem is that the equity of health is mostly not quantifiable due to lack of consistent and reliable methods of recording patient related profile or clinical information.
When Sankalp’s first thalassemia day care unit was established it was at a government institute. The economic status of many families was very bad and they came from several remote areas of the state. Therefore, right from 2011 we have aimed at creating a model where all steps required to ensure that the child is doing well medically is put in place.
Our thalassemia day care centers are powered by ThalCare. Capturing intense level of patient profile and clinical information is done as a matter of standard routine for all patients. Every visit is recorded and each test done, blood products transfused, medicines prescribed are all recorded for each patient. This makes it possible for us to investigate if there is any mismatch in the equity of care being provided.
We believe that this possibility to regularly view and analyze retrospective data has implicitly empowered the staff at the centers to achieve equity in delivery. It ofcourse also does involve external factors like support, counseling etc. If we were to take chelation as an example, we follow multiple strategies - full support , partial support , support through public healthcare schemes based on eligibility or encourage the family to bear the costs if it is financially viable for them. The baseline goal is to ensure that there is no iron overload to the degree that it can cause damage. Irrespective of how chelation is made available, we constantly review the ferritin levels of all patients to check if there are any trends indicating more intervention. The moment we realize that in successive determinations the child seems to be having disturbing levels of iron overload in the body, we initiate the next level of action. For several of them it could to start them on desferal therapy. This is done without creating any additional financial burden on the family. So here while the review, analysis, intervention techniques are all powered by ThalCare, strategies for support, making additional resources available are all external factors.
We embarked upon an exercise to assess the equity of care at 5 centres powered by ThalCare.All these centers are treating a minimum of 100 patients, and have nearly complete adoption of ThalCare for all patients in their centres. In total the assessment involved nearly 2500 patients.
It must also be noted that this assessment is from the time the center was operational. Therefore for some centers it has data for nearly 5 years and for the more recently opened ones data is available atleast for the last one year
There was no clinically significant difference observed in the equity of care as measured by average pre-transfusion haemoglobin levels between the two gender, the distance of the patient's house from the center, the age of the patients and the economic categorization of the patients. Girls outperformed the boys in most centers and patients managed to maintain haemoglobin levels across age groups in-spite of the increased blood requirements and frequent visits. Children coming from economically weaker families had marginally lower haemoglobin levels.
All centers saw a steadily dropping rate of mortality, which got limited to about 1% in last year. There was no significant difference in mortality based upon gender(p=0.48) ,distance the patient had to travel to reach the point of care (p=0.46) and whether or not splenectomy was done(p=0.35). The survival of patients from the families below poverty line was better than those above poverty line (p=0.036). This may party be explained by the fact that poorer families almost always had free chelators given by the center and thus had full compliance while those above the poverty line unlike the patients above poverty many of which were expected to party pay for their chelation therapy. The mortality varied very significantly with the age of enrollment at the center (p=0.003).37 patients were cured of ST with BMT while 4(10.8%) suffered from transplant related mortality..
A key challenge in the delivery of healthcare is maintaining equity across gender, religion, age, economic status and distance from the point. Post enrollment, there were no clinically significant differences observed in the access to care, which is in stark contrast to the prevalent situation in the country. While the gender ratio was highly skewed at enrollment, during the course of treatment the girls received care at par with the boys. In some centers, girls marginally outperformed the boys. We also noted that the difference in enrollment of girls and boys increased from metros, to tier to cities and was most striking for patients from smaller towns. There still remains a marginal difference between those below and above the poverty line. Loss of salary of the guardian for the day on which they bring the child for treatment may be contributing to this
While the results make us excited and helped us ascertain that equity of care is being addressed on most parameters, it also helped us identify gaps in our own centers.
We are happy that more centers are displaying an intent to adopt ThalCare for their operations.This gives us the confidence that in a few years time, the equity of care achieved in thalassemia management through ThalCare will be looked upon as a benchmark reference across the Indian healthcare domain.
