Thanks to the amazing success of the centres part of the Sankalp-Cure2Children network for Pediatric BMT, we are receiving more and more requests from families who have a thalassemic kid looking for the option of cure. While we do guide them on a case by case basis there are some key points which we have observed.
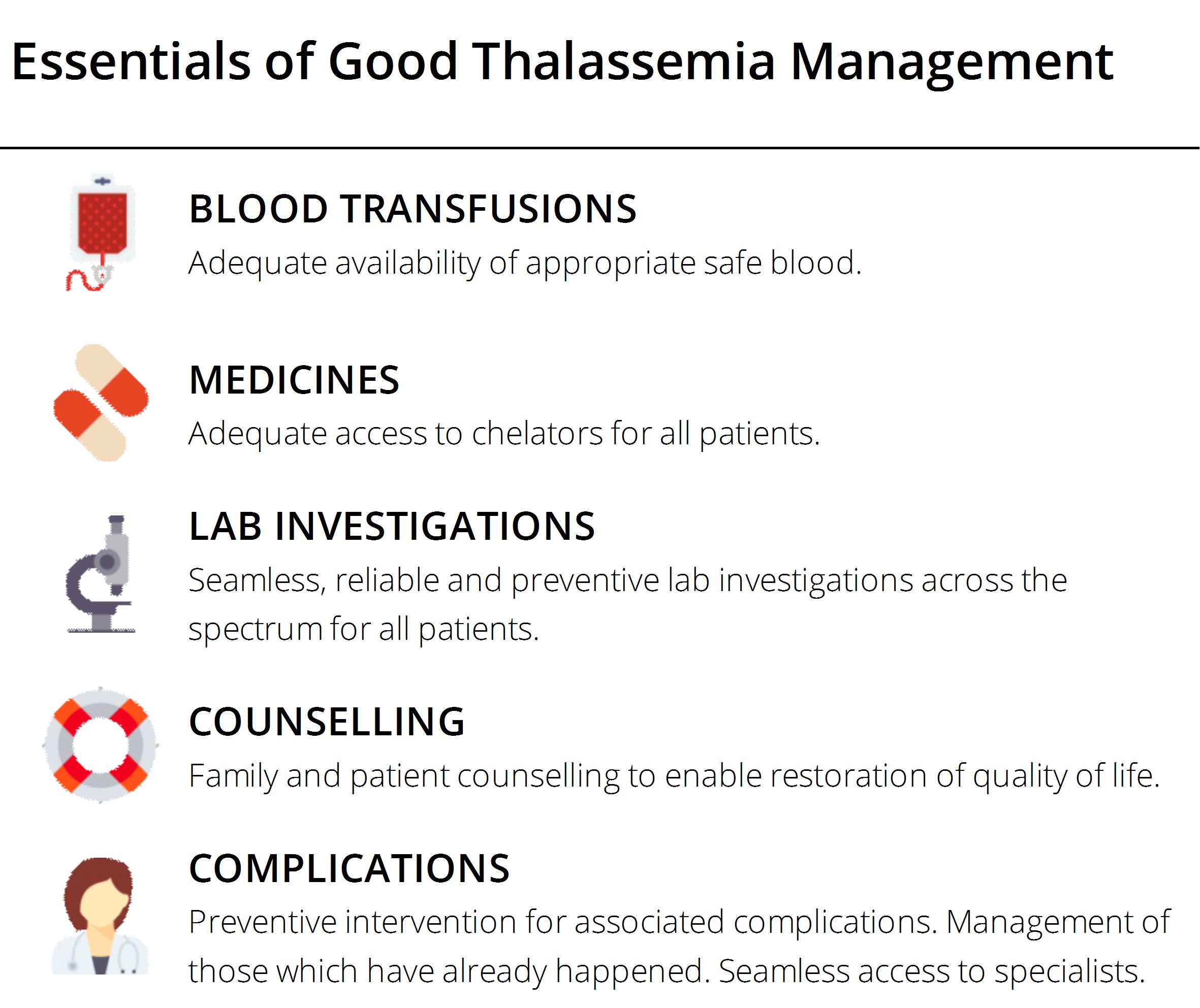
Most patients coming to seek advice for the curative option for transplantation are poorly chelated, have very low pre-transfusion haemoglobin levels, and have almost negligible monitoring of their growth and complications. It should be understood that even if a child has the best donor for transplantation (a fully matched sibling), still the child is less likely to do well with transplantation if the child is not in a good shape for it.
There are some systemic reasons for kids being in bad shape. The major one being lack of availability of good thalassemia centres for management. Fortunately, there is a greater push for better care and management for thalassemia and we have more centres which deliver comprehensive management. It is better to choose those centres even if they are at a distance than those who basically transfuse and send the child back.
The second problem is the emotional and economic fatigue the families go through when they are chronically managing the child with little hope for change in circumstances. Now, for most families, there is reasonable ground to say that their child may have a safe option of cure somewhere in near future. Haploidentical transplantations are catching pace and recent results show that they can be close to the matched sibling ones. These transplants use the mother or the father as the donor and thus almost all the thalassemia kids now may have a donor for the transplantation. Additionally, these Haploidentical transplantations promise to be safer than the unrelated donor transplantations. They are promising lesser graft versus host disease (a complication pretty common with unrelated donor transplantations which may make life worse than thalassemia) and even lesser mortality. Though it is difficult to call Haploidentical transplants the accepted standard of care already, the indicators look very promising.
With this hope right there, the support organisations, doctors and the parents themselves have good reason to be optimistic and engage fiercely in keeping their children in best shape.
Another issue to discuss is the pressure on parents to get one more baby "to cure" the affected child. Working with hundreds of thalassemia families closely and knowing the social dynamics, we at Sankalp advice the families to go for the next child if and only if they want the next child irrespective of whether he or she is a match with the first one. As it is the chance of a match is only 25%. What makes things worse is the fact that sometimes families are encouraged to take up illegal and unethical interventions like screening the foetus for a match and abort it in case of failure.
We should also briefly clarify our stand on the issue of saving cord blood of the future siblings. Inline with what is known, established and widely endorsed, we inform the families that there is no reason for them to save the stem cells of the child with the hope of using the same for a cure from thalassemia. Should the child be a match, bone marrow would be a preferred source. The unqualified, sometimes inappropriate hope given to the families by the people involved in the cord blood industry nudge them into spending huge amounts of money to secure cord blood - which essentially is of no good use to the patient.
As we see, in near future, pediatric patients who are well maintained have a good chance of getting cured of thalassemia whether or not they have a sibling donor. Staring now to get them in great shape looks like a major priority of the moment.
Sankalp India Foundation can be contacted for advice on Bone Marrow Transplantation for kids at contact@sankalpindia.net or +91-9480044444.
