With so much news about Ebola around it is important to maintain an up-to-date and accurate understanding of the disease. WHO fact sheet serves the purpose of providing accurate and reliable information about this disease outbreak. We share with you Fact sheet N°103 updated September 2014
Key facts
- Ebola virus disease (EVD), formerly known as Ebola haemorrhagic fever, is a severe, often fatal illness in humans.
- The virus is transmitted to people from wild animals and spreads in the human population through human-to-human transmission.
- The average EVD case fatality rate is around 50%. Case fatality rates have varied from 25% to 90% in past outbreaks.
- Community engagement is key to successfully controlling outbreaks. Good outbreak control relies on applying a package of interventions, namely case management, surveillance and contact tracing, a good laboratory service, safe burials and social mobilisation.
- Early supportive care with rehydration, symptomatic treatment improves survival. There is as yet no licensed treatment proven to neutralise the virus but a range of blood, immunological and drug therapies are under development.
- There are currently no licensed Ebola vaccines but 2 potential candidates are undergoing evaluation.
Background

The Ebola virus causes an acute, serious illness which is often fatal if untreated. Ebola virus disease (EVD) first appeared in 1976 in 2 simultaneous outbreaks, one in Nzara, Sudan, and the other in Yambuku, Democratic Republic of Congo. The latter occurred in a village near the Ebola River, from which the disease takes its name.
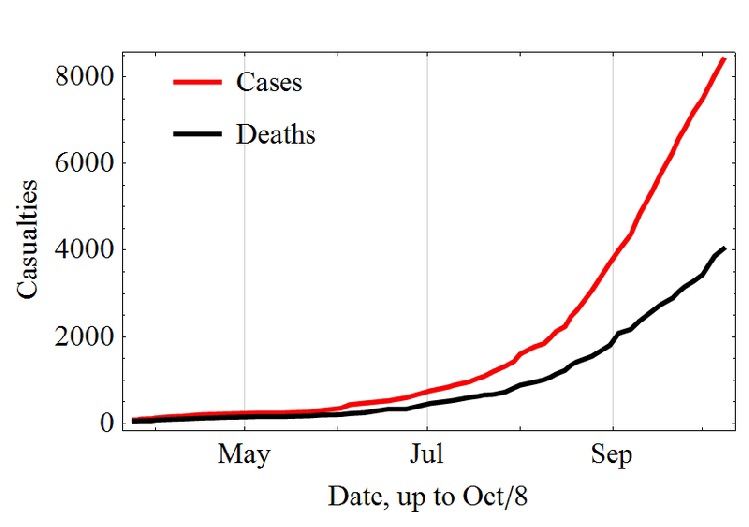
The current outbreak in west Africa, (first cases notified in March 2014), is the largest and most complex Ebola outbreak since the Ebola virus was first discovered in 1976. There have been more cases and deaths in this outbreak than all others combined. It has also spread between countries starting in Guinea then spreading across land borders to Sierra Leone and Liberia, by air (1 traveller only) to Nigeria, and by land (1 traveller) to Senegal.
The most severely affected countries, Guinea, Sierra Leone and Liberia have very weak health systems, lacking human and infrastructural resources, having only recently emerged from long periods of conflict and instability. On August 8, the WHO Director-General declared this outbreak a Public Health Emergency of International Concern.
Transmission
It is thought that fruit bats of the Pteropodidae family are natural Ebola virus hosts. Ebola is introduced into the human population through close contact with the blood, secretions, organs or other bodily fluids of infected animals such as chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the rainforest.
Ebola then spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD. This has occurred through close contact with patients when infection control precautions are not strictly practiced.
Burial ceremonies in which mourners have direct contact with the body of the deceased person can also play a role in the transmission of Ebola.
People remain infectious as long as their blood and body fluids, including semen and breast milk, contain the virus. Men who have recovered from the disease can still transmit the virus through their semen for up to 7 weeks after recovery from illness.
Symptoms of Ebola virus disease
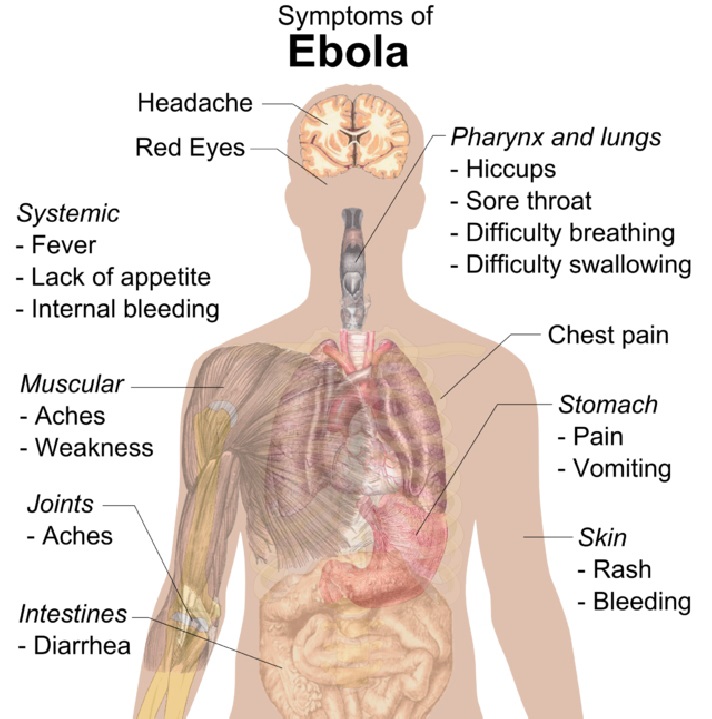
The incubation period, that is, the time interval from infection with the virus to onset of symptoms is 2 to 21 days. Humans are not infectious until they develop symptoms. First symptoms are the sudden onset of fever fatigue, muscle pain, headache and sore throat. This is followed by vomiting, diarrhoea, rash, symptoms of impaired kidney and liver function, and in some cases, both internal and external bleeding (e.g. oozing from the gums, blood in the stools). Laboratory findings include low white blood cell and platelet counts and elevated liver enzymes.
Diagnosis
It can be difficult to distinguish EVD from other infectious diseases such as malaria, typhoid fever and meningitis. Confirmation that symptoms are caused by Ebola virus infection are made using the following investigations:
- antibody - capture enzyme - linked immunosorbent assay (ELISA)
- antigen-capture detection tests
- serum neutralization test
- reverse transcriptase polymerase chain reaction (RT-PCR) assay
- electron microscopy
- virus isolation by cell culture.
Samples from patients are an extreme biohazard risk; laboratory testing on non-inactivated samples should be conducted under maximum biological containment conditions.
Treatment and vaccines
Supportive care-rehydration with oral or intravenous fluids- and treatment of specific symptoms, improves survival. There is as yet no proven treatment available for EVD. However, a range of potential treatments including blood products, immune therapies and drug therapies are currently being evaluated. No licensed vaccines are available yet, but 2 potential vaccines are undergoing human safety testing.
Prevention and control
Good outbreak control relies on applying a package of interventions, namely case management, surveillance and contact tracing, a good laboratory service, safe burials and social mobilisation. Community engagement is key to successfully controlling outbreaks. Raising awareness of risk factors for Ebola infection and protective measures that individuals can take is an effective way to reduce human transmission. Risk reduction messaging should focus on several factors:
- Reducing the risk of wildlife-to-human transmission from contact with infected fruit bats or monkeys/apes and the consumption of their raw meat. Animals should be handled with gloves and other appropriate protective clothing. Animal products (blood and meat) should be thoroughly cooked before consumption.
- Reducing the risk of human-to-human transmission from direct or close contact with people with Ebola symptoms, particularly with their bodily fluids. Gloves and appropriate personal protective equipment should be worn when taking care of ill patients at home. Regular hand washing is required after visiting patients in hospital, as well as after taking care of patients at home.
- Outbreak containment measures including prompt and safe burial of the dead, identifying people who may have been in contact with someone infected with Ebola, monitoring the health of contacts for 21 days, the importance of separating the healthy from the sick to prevent further spread, the importance of good hygiene and maintaining a clean environment.
Controlling infection in health-care settings
Health-care workers should always take standard precautions when caring for patients, regardless of their presumed diagnosis. These include basic hand hygiene, respiratory hygiene, use of personal protective equipment (to block splashes or other contact with infected materials), safe injection practices and safe burial practices.
Controlling infection in health-care settings
Health-care workers caring for patients with suspected or confirmed Ebola virus should apply extra infection control measures to prevent contact with the patient's blood and body fluids and contaminated surfaces or materials such as clothing and bedding. When in close contact (within 1 metre) of patients with EBV, health-care workers should wear face protection (a face shield or a medical mask and goggles), a clean, non-sterile long-sleeved gown, and gloves (sterile gloves for some procedures).
Laboratory workers are also at risk. Samples taken from humans and animals for investigation of Ebola infection should be handled by trained staff and processed in suitably equipped laboratories.
After thought
From a blood banking point of view there are multiple reasons to take early note of any pandemic/edipedemic that is being reported globally. In the connected world, disease travels faster than ever before. Right now is a good time for everyone in healthcare to devote some time and effort for disaster planning and preparedness. While we hope for the best, should the situation arise, how will our facilities respond to the challenge? The frequency of disasters is on the rise and the need for proper disaster mitigation and preparedness is like never before in history.
Clearly the simplest and easiest first steps in the direction of preparation is the adoption of rigorous hand hygiene and safe injection practice in - line with WHO recommendations.
Sankalp India Foundation offers whatever little expertise and experience the organisation has at disaster mitigation and response to any blood bank which is keen on establishing a well laid out protocol for emergency and disaster preparedness.
Source
http://www.who.int/mediacentre/factsheets/fs103/en/
Images taken from
Http://en.wikipedia.org/wiki/Ebola_virus_disease
